Visit Us Mon-Fri from 9:00 AM to 5:00 PM
401 Mall Blvd Ste 101-d, Savannah GA 31406
Visit Us Mon-Fri 9:00am - 5:00pm
What Is an Intensive Outpatient Program (IOP) and How Does It Support Mental Health and Addiction Recovery?
July 25, 2025, by New Day Counseling
More than 20 million Americans face the dual challenge of mental health disorders and addiction, yet many struggle to find treatment that combines structured care with day-to-day flexibility. An intensive outpatient program (IOP) bridges this gap by delivering concentrated therapy sessions without requiring overnight stays, allowing participants to maintain work, school, or family responsibilities while receiving evidence-based interventions. In this guide, you will discover:
1. What defines an IOP and how it differs from other outpatient therapies
2. The specific conditions addressed and the mechanics behind dual diagnosis treatment
3. Core benefits such as flexibility, cost efficiency, and community integration
4. Comparisons with inpatient and partial hospitalization care
5. A detailed breakdown of the typical IOP experience, including schedules and counselor roles
6. Strategies for finding, evaluating, and financing an IOP near you
7. Data on success rates, patient testimonials, and long-term recovery support
Together, these sections form a complete roadmap to understanding how an intensive outpatient program empowers individuals on their journey to mental wellness and addiction recovery.
What Is an Intensive Outpatient Program (IOP)?
An intensive outpatient program (IOP) is a structured non-residential treatment modality that provides 9–19 hours of weekly therapy to treat mental health disorders and substance use disorders, integrating individual, group, and family sessions. This framework leverages evidence-based modalities like CBT and DBT to build coping skills, relapse prevention strategies, and psychoeducation in a community setting. For example, someone with moderate depression might attend three group therapy sessions per week while continuing work responsibilities. Defining IOP as a mid-level treatment option sets the stage for exploring how it differs from traditional outpatient therapy.
How Does IOP Differ from Traditional Outpatient Therapy?
IOP delivers a higher intensity of care than standard weekly counseling by combining multiple modalities in a concentrated schedule over several weeks. Traditional outpatient therapy typically involves one individual session per week, whereas an IOP schedules three to five sessions per week, each lasting 2–3 hours, to accelerate skill acquisition and peer support.
~ Entity: Therapy Intensity → Attribute: Sessions per Week → Value: 3–5
~ Entity: Session Duration → Attribute: Time → Value: 2–3 hours
~ Entity: Patient Engagement → Attribute: Activities → Value: Group, individual, family interventions
By layering these components, IOP ensures more frequent reinforcement of coping strategies, which contrasts with the slower pace of standard outpatient care and naturally leads into an examination of IOP’s core components.
What Are the Core Components of an IOP?
An IOP’s core components integrate multiple therapeutic approaches in a cohesive framework designed to treat complex needs:
1. Group Therapy: Facilitates peer support and shared coping strategies through guided discussions.
2. Individual Therapy: Delivers personalized goal-setting, cognitive restructuring, and relapse prevention planning.
3. Family Therapy: Strengthens communication patterns and address systemic dynamics influencing recovery.
4. Psychoeducation: Provides evidence-based knowledge about disorders, triggers, and healthy coping mechanisms.
5. Skill-Building Workshops: Teach DBT emotion regulation, mindfulness, and stress management techniques.
These components work together to address emotional regulation, social support, and practical life skills, forming a comprehensive treatment package that naturally transitions to eligibility criteria.
Who Is Eligible for IOP Treatment?
Individuals who require a more intensive level of support than weekly therapy but do not need 24/7 supervision are ideal IOP candidates, including:
~ Adults and adolescents with moderate to severe depression or anxiety
~ Individuals in early recovery from alcohol or drug dependence requiring structured relapse prevention
~ Patients transitioning from inpatient or partial hospitalization care as a step-down option
~ People with co-occurring disorders who benefit from integrated mental health and addiction interventions
Meeting ASAM criteria for Level 2.1, eligibility reflects clinical necessity and the ability to manage self-care outside the treatment setting, setting up the next discussion on conditions addressed.
What Conditions Are Treated in an Intensive Outpatient Program?
IOP treats a range of mental health and substance use disorders by applying targeted therapeutic modalities to each condition with proven efficacy. Understanding these condition clusters clarifies how treatment plans are tailored.
How Does IOP Address Substance Use Disorders?
An IOP for substance use disorders provides focused relapse prevention, coping-mechanism training, and group support to maintain sobriety.
~ Entity: Alcohol Use Disorder → Attribute: Treatment Focus → Value: Craving management and peer accountability
~ Entity: Opioid Use Disorder → Attribute: Therapy Modality → Value: Motivational interviewing and contingency management
~ Entity: Relapse Prevention → Attribute: Techniques → Value: Cue exposure and coping skills rehearsal
This integrated approach reduces risk of return to use and introduces the complementary exploration of mental health disorder treatments.
How Does IOP Support Mental Health Disorders?
IOP employs tailored interventions for mental health challenges, combining cognitive and behavioral therapies with skills training to alleviate symptoms.
~ Entity: Major Depressive Disorder → Attribute: Modality → Value: CBT for negative thought patterns
~ Entity: Generalized Anxiety Disorder → Attribute: Strategy → Value: Mindfulness and exposure exercises
~ Entity: Trauma-Related Disorders → Attribute: Technique → Value: EMDR elements within group processing
These targeted strategies enhance emotional regulation and resilience, paving the way to dual diagnosis treatment discussion.
What Is Dual Diagnosis Treatment in IOP?
Dual diagnosis treatment in IOP integrates simultaneous care for co-occurring mental health conditions and substance use disorders, ensuring neither issue is treated in isolation. Interventions include:
~ Coordinated Case Management to synchronize therapy goals across conditions
~ Integrated Group Sessions blending relapse prevention with trauma-informed care
~ Collaboration Between Counselors (substance abuse counselor, certified addiction counselor, drug alcohol counselor) to create unified treatment plans
By treating both disorders concurrently, dual diagnosis IOP enhances overall outcomes and prepares the ground for exploring program benefits.
Effectiveness of Dual Diagnosis Treatment
Dual diagnosis treatment within IOPs, which addresses co-occurring mental health and substance use disorders simultaneously, has been shown to improve overall outcomes. Integrated treatment models, including coordinated case management and collaborative therapy sessions, lead to better results than treating each condition separately.
National Institute on Drug Abuse, "Principles of Drug Addiction Treatment: A Research-Based Guide" (2018)
This citation supports the article's discussion of dual diagnosis treatment and its benefits within the IOP framework.
What Are the Benefits of an Intensive Outpatient Program?
IOP delivers a blend of structured care and real-world application, generating multiple advantages over other treatment settings. Recognizing these benefits illustrates why IOP often becomes the preferred level of care.
How Does IOP Provide Flexibility for Patients?
IOP’s non-residential design allows participants to maintain employment, education, and family roles while attending therapy sessions several days per week.
1. Retains daily responsibilities without interruption.
2. Encourages immediate practice of coping skills in natural environments.
3. Minimizes stigma by preserving community integration.
Benefits of Intensive Outpatient Programs
Intensive Outpatient Programs (IOPs) offer a flexible approach to mental health and addiction treatment, allowing individuals to maintain their daily routines while receiving structured therapy. This flexibility is a key advantage over inpatient care, enabling patients to integrate new coping skills into their real-world environments and minimize disruptions to their lives.
SAMHSA, "What is an Intensive Outpatient Program?" (2024)
This research supports the article's claims about the flexibility and benefits of IOPs compared to more restrictive treatment settings.
This flexibility underpins IOP’s cost-effectiveness when compared to residential care.
Why Is IOP Considered Cost-Effective Compared to Inpatient Care?
By eliminating room and board expenses and reducing staffing overhead, IOP generally costs 40–70 percent less than inpatient treatment while delivering comparable therapeutic intensity.
~ Entity: Cost Category → Attribute: Inpatient Care → Value: High (includes lodging, meal services)
~ Entity: Cost Category → Attribute: IOP → Value: Moderate (therapy-only expenses)
~ Entity: Insurance Coverage → Attribute: Typical Coverage → Value: 80–100 percent for medically necessary IOP
Lower out-of-pocket costs enhance treatment accessibility and lead into how IOP fosters community support.
How Does IOP Promote Community Integration and Support?
An IOP leverages group cohesion and real-life skill application to build robust peer networks and practical problem-solving.
~ Entity: Peer Support → Attribute: Impact → Value: Increased accountability and reduced isolation
~ Entity: Skill Application → Attribute: Context → Value: Real-world stressors addressed in therapy
~ Entity: Community Resources → Attribute: Linkages → Value: Local support groups and vocational services
This community focus sets the stage for comparing IOP with other care levels.
How Does an Intensive Outpatient Program Compare to Other Levels of Care?
Positioning IOP within the continuum of care clarifies its ideal role as either a step-down from more intensive settings or a step-up when weekly therapy is insufficient.
What Are the Differences Between IOP and Inpatient Treatment?
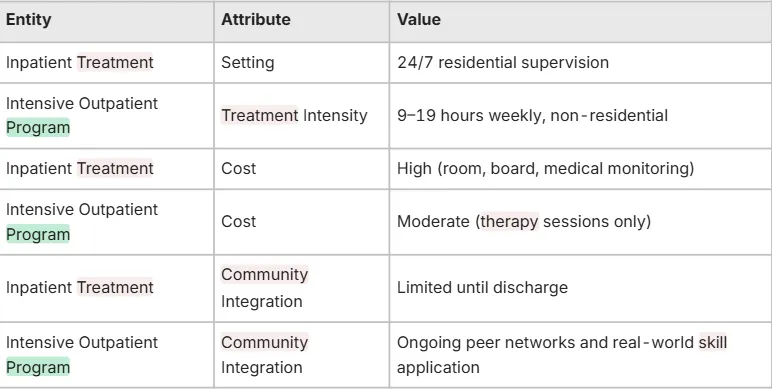
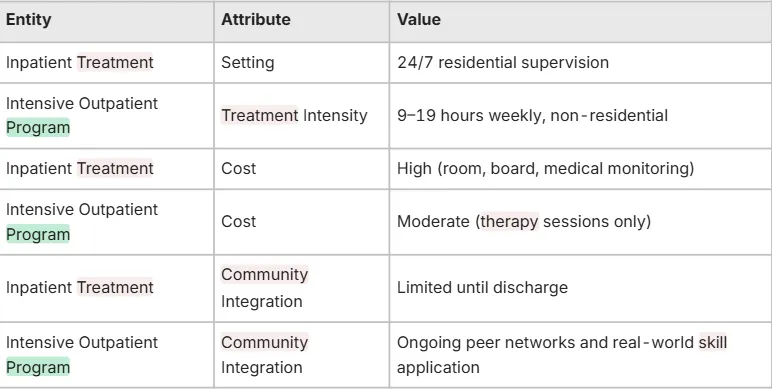
This community focus sets the stage for comparing Positioning IOP within the continuum of care clarifies its ideal role as either a step-down from more intensive settings or a step-up when weekly therapy is insufficient.
IOP with other care levels.
How Does IOP Compare to Partial Hospitalization Programs (PHP)?
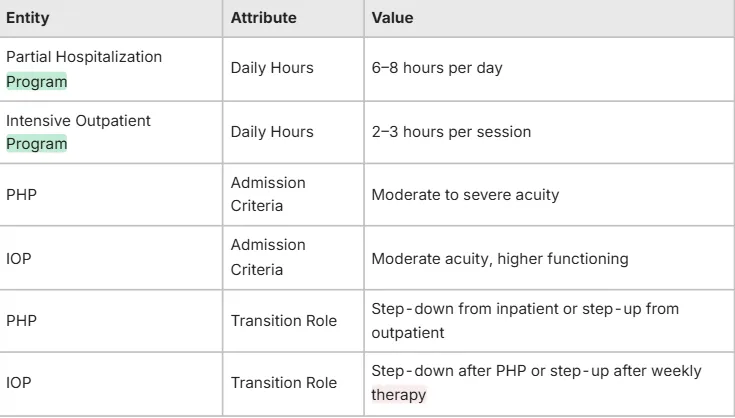
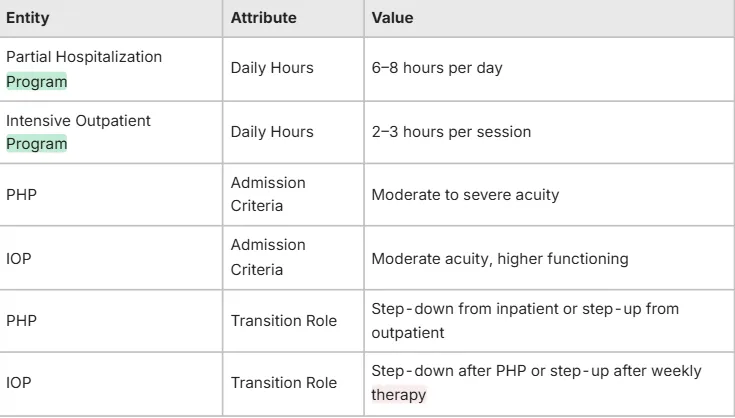
Understanding these distinctions sets up when to use IOP as a step-down or step-up option.
When Is IOP Used as Step-Down or Step-Up Care?
IOP serves as a bridge:
~ Step-Down: Following stabilization in inpatient or PHP to reinforce skills in real life.
~ Step-Up: When weekly outpatient therapy fails to manage symptoms or cravings adequately.
This strategic positioning underscores IOP’s versatility and leads directly into the typical participant experience.
What Is the Typical Experience in an Intensive Outpatient Program?
Knowing what a day in IOP looks like helps set expectations and ease transitions into treatment.
What Does a Daily IOP Schedule Look Like?
A typical IOP day balances group sessions, individual counseling, and skills workshops over 3 hours:
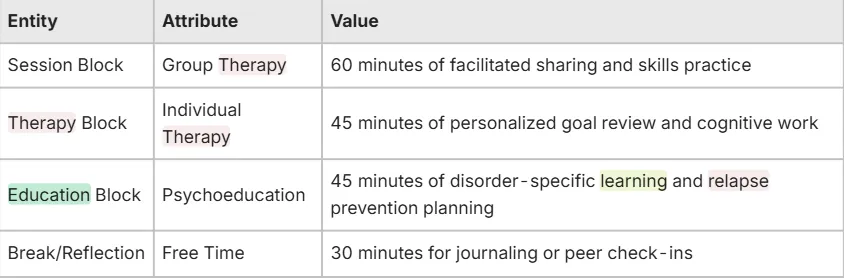
This structured schedule leads to exploring the specific therapies offered within IOP.
What Types of Therapy Are Offered in IOP?
IOP typically includes:
Cognitive Behavioral Therapy (CBT) to reframe negative thought patterns
Dialectical Behavior Therapy (DBT) for emotion regulation and distress tolerance
Motivational Interviewing to enhance readiness for change
Family Systems Therapy to repair relational dynamics
Mindfulness-Based Stress Reduction to cultivate present-moment awareness to repair relational dynamics
These modalities combine under a unified treatment plan, showing how substance abuse counselors and certified addiction counselors implement these approaches.
What Role Do Substance Abuse Counselors and Certified Addiction Counselors Play?
Substance abuse counselors and certified addiction counselors design and facilitate treatment components, including:
1. Assessment and Treatment Planning to set personalized goals.
2. Group Facilitation to guide peer-support exercises and skill practice.
3. Individual Counseling to reinforce relapse prevention techniques.
4. Case Coordination to connect clients with community resources.
Their expertise ensures cohesive care, preparing participants for alternative delivery formats like virtual IOP.
How Does a Virtual Intensive Outpatient Program Work?
A virtual IOP replicates in-person intensity through secure video platforms, offering:
~ Live group and individual sessions via HIPAA-compliant telehealth
~ Digital psychoeducation modules and interactive workshops
~ Online peer support forums moderated by certified addiction counselors
~ Remote monitoring of homework and progress tracking
Virtual delivery preserves core therapeutic mechanisms while increasing accessibility, leading to questions on how to select the right program nearby.
How Can I Find and Choose the Right Intensive Outpatient Program Near Me?
Selecting the best IOP involves evaluating location, specialization, and accreditation to match individual needs.
What Factors Should I Consider When Selecting an IOP?
Key considerations include:
Specialization: Expertise in your primary concern (e.g., trauma-informed care, substance abuse)
Accreditation: Joint Commission or CARF certification indicating quality standards
Therapist Credentials: Presence of licensed substance abuse counselors and certified addiction counselors
Group Composition: Demographics and disorder-specific focus aligning with your profile
Evaluating these factors ensures a program that aligns with clinical goals and naturally leads into financing considerations.
How Do IOP Costs and Insurance Coverage Affect My Options?
Cost transparency requires assessing:
Program Fees: Sliding-scale versus fixed rates per week
Insurance Benefits: In-network coverage for medical necessity, copays, and prior authorization requirements
Out-of-Pocket Estimates: Based on projected weekly hours and insurance reimbursements
Understanding financial responsibilities informs realistic planning and transitions into exploring virtual service availability.
Where Can I Access Virtual or Online IOP Services?
Remote IOP services are increasingly available through:
~ Telehealth platforms affiliated with licensed treatment centers
~ Specialized virtual clinics offering disorder-specific tracks
~ Community mental health providers expanding into digital care
By verifying credentials, technology security, and session structure, you can select a virtual IOP that fits your lifestyle and paves the way to assessing outcomes.
What Are the Success Rates and Patient Outcomes of Intensive Outpatient Programs?
Evaluating effectiveness and real-world results builds confidence in choosing IOP as a treatment approach.
What Do Patient Testimonials Reveal About IOP Effectiveness?
Patient testimonials often highlight:
Improved Coping Skills: Participants credit IOP for teaching practical relapse prevention techniques.
Enhanced Emotional Regulation: Many report reduced anxiety and depressive symptoms within weeks.
Sustainable Peer Networks: Graduates maintain support groups formed during IOP.
These firsthand accounts illustrate measurable benefits and lead into long-term recovery support mechanisms.
How Does IOP Support Long-Term Recovery and Relapse Prevention?
IOP fosters lasting change through:
Coping Skill Mastery reinforced in real-life contexts.
Ongoing aftercare referrals to alumni groups and community resources.
Periodic check-in sessions for early detection of relapse indicators.
By embedding relapse prevention into daily routines, IOP lays a foundation for sustained wellness beyond the program’s end.
An intensive outpatient program blends structured, evidence-based therapy with the flexibility of home-based living, offering a balanced approach to mental health and addiction recovery. Its capacity to integrate multiple modalities, foster community support, and adapt to individual schedules makes IOP a versatile option across the continuum of care. From clear comparisons with inpatient and PHP models to detailed schedules and counselor roles, understanding IOP provides a comprehensive framework for choosing the right level of care. With strong success rates and patient-driven testimonials, IOP stands as an effective step toward long-term resilience and relapse prevention.

PARENT COMPANY:
CREATIVE COUNSELLING SOLUTIONS LLC.
We Work for You Mon-Fri
from 9:00 AM to 5:00 PM
QUICK LINKS
© 2025 NEW DAY COUNSELING. All Rights Reserved.